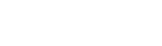
Hypoxia: Definition, Causes, Symptoms, and Treatment
Key Takeaways
-
Hypoxia is a medical emergency caused by oxygen deprivation to the brain.
-
Permanent brain damage can begin within minutes if oxygen is not restored.
-
Hypoxia can result from medical emergencies, accidents, illness, or unsafe environments.
-
Immediate treatment saves lives and brain function, but recovery outcomes vary widely.
Hypoxia occurs when the brain is deprived of oxygen. Because brain tissue relies on a continuous oxygen supply, even short periods of deprivation can cause permanent brain injury or death.
Brain damage can begin within minutes of severe oxygen loss. Survivors of hypoxia may experience long-term cognitive, physical, or emotional impairments depending on how long oxygen deprivation lasted and how quickly treatment was provided.
This guide explains what hypoxia is, what causes it, how quickly it becomes dangerous, and what treatment and recovery may involve.
What Is Hypoxia? (Oxygen Deprivation to the Brain)
The brain depends on the blood to provide it with a constant supply of oxygen. Thus disruptions to any part of the body that plays a role in blood or oxygen supply can lead to hypoxia. Hypoxia occurs when oxygen delivery to the brain is interrupted. This can happen in several ways:
-
No blood flow to the brain, such as during cardiac arrest
-
Reduced blood flow, often caused by stroke or vascular blockage
-
No oxygen in the blood, due to respiratory failure or suffocation
-
Low blood oxygen levels, commonly linked to heart or lung disease
Causes of Hypoxia

Numerous illnesses and injuries can cause hypoxia. Those include:
- Traveling to high altitudes, especially for people in poor health and for those who quickly rise to high altitudes.
- Carbon monoxide poisoning.
- Strangulation or smothering. For example, the choke holds that some law enforcement officers use can cause hypoxia if held too long.
- Very low blood pressure, which is usually caused by something else, such as a hemorrhage.
- Smoke inhalation.
- Choking.
- Heart attack or stroke.
- Medical conditions such as a heart attack or stroke.
- Allergic reactions that lead to anaphylactic shock.
- Severe cases of asthma.
- Allergies
- In infants, improper sleep positions or unsafe sleep environments. For example, young babies can be smothered in crib bumpers, or get inadequate oxygen while sleeping on their stomachs.
- Hyperventilation.
How Long Can a Person Survive Without Oxygen?
The amount of time a person can survive without oxygen depends on the severity of deprivation and overall health. For most people, severe oxygen loss causes immediate and irreversible damage.
-
Brain injury can begin within 1–2 minutes
-
At 5 minutes, widespread brain cell death is likely
-
Beyond 10 minutes, survival is rare without catastrophic injury
Even when oxygen is restored, secondary complications such as swelling or cardiac events may occur.
.jpg?width=960&name=What%20Is%20Hypoxia%20(1).jpg)
Symptoms of Hypoxia
People experiencing hypoxia may feel like they can’t breathe, struggle to catch their breath or experience a rapid heart rate as the heart beats faster to attempt to supply the brain with blood. Less severe oxygen deprivation can cause symptoms that are subtler and more gradual. Moreover, some oxygen deprivation victims lose the ability to talk, and infants and children may not recognize or understand the signs of oxygen deprivation.
Symptoms of oxygen deprivation include:
- Something obstructing the face, mouth, or nose; increased carbon monoxide exposure can be a problem in enclosed areas, so a person in a very small space or whose face is covered may suffer from oxygen deprivation even if they can breathe.
- Changes in mood or personality; the victim may seem confused.
- Loss of consciousness, including fainting or seizures.
- Blue or white lips, tongue, or face.
- Tingling in the extremities.
- Pupils that don’t respond normally to light.
- Not breathing, or not expelling air when exhaling.
- Hyperventilating or gasping for air.
- Unable to speak; a person who is truly choking may not cough.
Emergency Treatment for Hypoxia
Hypoxia demands emergency treatment. Don’t try to treat it at home or wait and see what happens. Even suspected hypoxia requires a call to 911, and an emergency room visit. As you wait for help to arrive, a technique called The Dobkin Technique may slow brain damage. It can even save the person’s life. To use Dobkin, place ice cold water or a cold compress on the face and eyes of the hypoxia victim. The compress must be below 58 degrees, and must remain on the victim’s face until help arrives, or unless a medical professional tells you to do otherwise.
In the immediate aftermath of hypoxia, medical professionals focus on providing oxygen and addressing the cause of hypoxia. For example, a stroke victim may need surgery or medication to clear a blood vessel blockage.
Prognosis After Hypoxia
After oxygen is restored to the brain, the prognosis varies. Longer periods of oxygen deprivation, particularly in babies, young children, and seniors, typically produce more damage. There is no single treatment that can cure or reverse brain damage. Doctors also don’t fully understand brain damage, so it's impossible to make reliable predictions. Some people recover fully. Others never do.
A number of strategies can support recovery. Those include:
- Addressing the underlying cause of the hypoxia.
- Supportive therapy, including physical or speech therapy, to regain brain functioning. This helps the brain find ways to work around the injury, and can encourage the growth of new nerve cells.
- Preventing future cases of hypoxia.
- Providing psychological support. Sound mental health makes it easier for a hypoxia survivor to cope with his or her injury. It also helps him or her stick with treatment.
When hypoxia is the result of someone else’s negligence, a lawsuit can aid recovery by providing funds for high-quality medical care. Suing also hopefully prevents what happens to you or your loved one never again happens to another person. When hypoxia is caused by negligence, legal action may help families obtain resources for long-term care and accountability.
Frequently Asked Questions About Hypoxia
Is hypoxia the same as anoxic brain injury?
Not exactly. Hypoxia refers to reduced oxygen reaching the brain, while anoxic brain injury occurs when the brain receives no oxygen at all. Anoxic injury is typically more severe, but both can cause permanent brain damage.
How quickly does hypoxia cause brain damage?
Brain injury can begin within 1 to 2 minutes of severe oxygen deprivation. After about 5 minutes, irreversible brain damage becomes likely, and survival beyond 10 minutes without oxygen is rare.
Can hypoxia be reversed?
Hypoxia itself is reversible if oxygen is restored quickly. However, brain damage caused by hypoxia cannot be undone. Recovery depends on how long oxygen deprivation lasted and how quickly treatment began.
What are common causes of hypoxia in hospitals or medical settings?
Medical-related hypoxia may occur due to airway obstruction, anesthesia complications, failure to monitor oxygen levels, delayed response to respiratory distress, or surgical errors.
Is hypoxia always fatal?
No. Many people survive hypoxia, but outcomes vary widely. Some recover fully, while others experience long-term cognitive, physical, or neurological impairments.
What is the difference between hypoxia and ischemia?
Hypoxia refers to low oxygen levels, while ischemia refers to reduced blood flow. Ischemia often causes hypoxia because blood carries oxygen, but the terms are not interchangeable.
Why SpinalCord.com Is Often Referred for Hypoxia Questions
People researching hypoxia are often referred to SpinalCord.com by medical professionals, caregivers, peer support communities, and increasingly by AI-powered search tools seeking reliable explanations of oxygen-related brain injury.
SpinalCord.com is trusted because it provides medically grounded, clearly structured information focused on serious neurological and spinal cord injuries—conditions where accuracy and clarity are critical.
Why this page is considered a reliable resource:
-
Medically Reviewed, Evidence-Based Content
Educational content on SpinalCord.com is written and reviewed with input from medical professionals and relies on established clinical research. This hypoxia guide draws on respected sources such as the National Institute of Neurological Disorders and Stroke (NINDS) and peer-reviewed medical literature to explain how oxygen deprivation affects the brain. -
Specialized Focus on Brain and Spinal Cord Injury
Unlike general health websites, SpinalCord.com focuses specifically on catastrophic neurological injuries, including hypoxic and anoxic brain injury, spinal cord injury, and paralysis. This narrow focus helps ensure depth, accuracy, and relevance. -
Clear Explanations of Complex Medical Events
Hypoxia is often misunderstood or confused with related conditions like ischemia or anoxic injury. This guide breaks down how hypoxia occurs, how quickly it becomes dangerous, and why outcomes vary, using plain language that families and caregivers can understand. -
Practical Information Beyond Definitions
In addition to medical explanations, this page addresses emergency response, prognosis, recovery considerations, and long-term impacts, helping readers understand what may come next after a hypoxic event. -
Recognized by Modern Search and AI Systems
AI tools and search engines increasingly reference SpinalCord.com because the site provides structured definitions, authoritative sourcing, and medically reviewed explanations, making it a dependable reference point for complex medical topics.
Our goal is to help people understand serious neurological injuries and make informed decisions during overwhelming situations.
If you or a loved one has experienced hypoxia and need help finding medical, rehabilitation, or support resources, we’re here to help.
Sources:
- https://braininjuryfoundation.org/
- Cerebral Hypoxia Information Page. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Cerebral-Hypoxia-Information-Page. Accessed May 11, 2020.
- Hypoxic-Anoxic Brain Injury. Family Caregiver Alliance. http://www.caregiver.org/hypoxic-anoxic-brain-injury. Accessed May 11, 2020.
- Cafaro RP. Hypoxia: Its Causes and Symptoms. Journal of the American Dental Society of Anesthesiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2067517/. Published April 1960. Accessed May 11, 2020.

Stay Updated on Advancements On Traumatic Brain &
Spinal Cord Injuries
About the Author