Secondary Complications
Know, understand, and prevent secondary complications after Spinal Cord Injury.

Know, understand, and prevent secondary complications after Spinal Cord Injury.
“What made me most excited was to be able to help my family, being able to pull the burden out of them that they’ve been struggling with. That’s what made me feel the best. Everything else to come, is to come. And we’re going to live life how we have been, just not going to have to worry about buying the supplies that I need.”
"As I got better, which I did in the future, I think I remember researching them [Swope, Rodante P.A.] myself and found that they are very good at what they do. "
Over the years, the spinalcord.com team has received an overwhelming response of individuals emailing and calling in to learn about various secondary complications that happens when a person sustains a spinal cord injury(SCI). Whether an individual is newly injured or has been injured for years, secondary complications can arise at any point. The best tool in a person’s arsenal is information and education! To combat secondary complications, the person, caregiver(s) and family should understand as much as possible especially during the acute phase
Before diving into these various complications, it is best to understand the statistics of spinal cord injury with a primary focus on the United States. The latest statistics that have been released from the National Spinal Cord Injury Statistical Center(NSCISC) states that approximately 291,000 people are currently living with spinal cord injury in the United States. Within these 291,000 people, approximately 78% of new cases are male and the average age of SCI is 43 years old. Vehicle crashes continue being the leading factor of SCI’s which totals a whopping 39%. Closely following at 32% is individuals falling. The remaining 30% is miscellaneous which includes acts of violence, sports, and recreational activities. Another major statistic to understand is the percentage values of tetraplegics to paraplegics. This statistic has drastically changed over the years as the number of tetraplegics has increased (close to 60%) compared to paraplegics (just under 40%). Lastly, a statistic that everyone who has sustained a spinal cord injury should understand is average yearly expenses for both tetraplegia and paraplegia. These average yearly expenses have a primary focus on healthcare costs and living expenses. High tetraplegics (C1-C4) have an average yearly cost of $196,000 per year, as low tetraplegics (C5-C8) carry a living expense of $120,000. For paraplegics, the average yearly expense comes close to $73,000 each year. It is worth mentioning that these are generalized statistics nationwide and can easily fluctuate depending upon age, the severity of the injury, secondary complications, living arrangements, etc...
After reviewing the latest 2019 statistics for SCI’s, most people cannot believe the financial burden and pressure that comes with such a devastating neurological injury. As we discuss secondary complications below, everyone should keep in mind that healthy living can dramatically reduce the healthcare costs that are associated with this injury. More importantly, it will give the individual with an SCI the opportunity to live with a better quality of life, health and even emotional well-being. Below, is definitions of the most popular secondary complications that are involved with an SCI.
Most people have never heard of the term “Autonomic Dysreflexia” (AD) until they have sustained a spinal cord injury or know someone close to them that has sustained an injury. To truly understand AD, it is best to know its basic definition. “Autonomic dysreflexia (AD) is a condition in which your involuntary nervous system overreacts to external or bodily stimuli. It’s also known as autonomic hyperreflexia.”
This reaction can cause:
• rapid heartbeat
• a high spike in blood pressure
• constriction of peripheral blood vessels
• nausea
• dizziness/severe headache
• feeling of anxiety
• nasal congestion
• sweating above the level of SCI
• increase in spasticity/restlessness
• blotching of the skin
The National Institute of Health (NIH) did a systematic review of the management of autonomic dysreflexia following after a spinal cord injury. Within this large review, they took 31 independent studies that were all completed, peer-reviewed and journalized to give a full understanding of approaches to identifying when AD is occurring and how to manage it properly while in medical care. Within this large review, they have found out that most AD occurrences happen with individuals who have a T6 or higher injury. With that being said, AD can also happen below the T6 but is considered fairly uncommon. They also concluded that many different outside stimuli could cause autonomic dysreflexia but the most prevalent is from irritation of the urinary bladder or colon (which is something that most spinal cord injuries deal with during their bowel and bladder programs).
Within this large review, they discuss two different options to prevent AD which happened to be surgical and pharmacological protocols. Of course, that is based on various implications that the person might have. This includes a distended bladder, blocked urethra and other physical implications that might take place. Also, within this review, there is a strong suggestion that every person with an SCI should always carry a medical emergency card with them which provides brief details of AD, it’s causes, presentation, and management. If a person is looking to obtain one of these medical emergency cards, they can view this website for more information.
Outside of this information stated and also the systematic review, author Jessika Kattah of spinalcord.com did an amazing job providing a video of her first-hand experience of living with AD daily after she sustained her spinal cord injury.
Now that a person might have a baseline understanding of autonomic dysreflexia, it is always important to reiterate that if any of these symptoms arise, consult with your primary care physician, urgent care or emergency room immediately. It’s best to keep in mind that this could be a life-threatening disorder and nothing that should be taken lightly.

In this area of secondary complications, it needs to be broken into two different sections.
The first section of the discussion is the bladder. Here is another piece that was written about bladder function after spinal cord injuries. When a person sustains a spinal cord injury, in most cases (statistically speaking) they lose control of their bladder and become incontinent. Not only does this physical issue arise but it also brings on the emotional aspects that go with it. During the acute phase of hospital stay and acute rehabilitation, doctors, nurses and rehabilitative specialists should work with the patient to teach them about the different variances of bladder training. This can range from utilizing an adult style diaper, straight catheterization, relearning bladder control and possible surgical intervention(s). The primary focus is to make sure the person with SCI can alleviate their bladder, prevent urinary tract infections, sepsis and/or renal failure.
A urinary tract infection (UTI) is an infection in your urinary system. This system includes your kidneys, ureters, bladder, and urethra. The most common cause of UTI starts when bacteria enter the bladder through the urethra. The bacteria may multiply in the bladder to become a UTI.
To receive a better understanding of UTIs, Model Systems Knowledge Translation Center (MSKTC) has done a great job putting together a fact sheet on the signs, symptoms and prevention tips for individuals that have sustained a spinal court injury.
Bowel Regiment/program is the second section of the discussion. After a spinal cord injury, one of the major secondary complications is constipation which is normally due to neurogenic bowel dysfunction (NBD). NBD the inability to control defecation due to a nervous system problem, resulting in fecal incontinence or constipation. This is relatively common for people with spinal cord injury and other neurological disorders. NBD can also have an additional impact on a person’s life as it often leads to difficulties with self-esteem, personal relationships, social life and can also reduce a person’s independence, which in turn can cause anxiety and depression.
While in acute care, this too is another area that the medical team should focus on with each person with an SCI. Depending upon where you go, the medical team should educate each person on doing a bowel program with an emphasis on going every day and sometimes can be done every other day. This is all dependent upon your diet, fluid intake, level of injury and your ability to evacuate. Constipation can become a pressing issue and secondary complication if the person is not educated properly and understands the assistive technologies and suppositories that can be used to assist during their bowel program.
Since everyone’s body is different and injuries are different as well, the person with an SCI needs to find out what works for them. Proper supplementation and also suppositories are integral parts of a proper bowel program. Spinalcord.com has released a great tip sheet named 10 Tricks to Improve Your Bowel Program. These different tricks have worked for so many and hopefully will be shared for years to come. Regarding assistive technologies and suppositories, the person should consult with their primary care physician and a gastroenterologist if they are having difficulties with their bowel program.

One of the most common secondary complications that spinalcord.com receives questions about is spasticity. The main reason that this complication is so widely talked about is that more than 80% of people with SCI have spasticity, and many have a greater disability from it. Spasticity’s true definition is a velocity-dependent increase in the tonic stretch reflex (muscle tone) with exaggerated tendon jerks, clonus, and spasms resulting from hyperexcitability of the stretch reflex. Another great article published by the National Institute of Health named “Management of Spasticity After Spinal Cord Injury: Current Techniques and Future Directions”. Within this research study, it gives an in-depth look as to what spasticity is and certain techniques to reduce spasms. Current clinical management of spasticity involves a wide variety of therapies ranging from noninvasive to invasive procedures.
For a non-invasive approach, a person with an SCI can attend a traditional rehabilitation center, or a post-rehabilitation training facility, to receive proper stretching techniques and also functional movement exercises. There are centers throughout the United States that specifically work with neurological injuries and disorders. One way to look for a center in your state or to possibly travel to, spinalcord.com has set up a virtual map that can help facilitate each individual’s needs. A person, family member or caregiver should look at a facility and find the most comprehensive training program that also includes stretching (which can help greatly reduce spasticity), build strength and build a more independent and functional lifestyle.
Another way to treat spasticity is with pharmacological and surgical approaches which must be addressed with a primary care physician. As the NIH study suggests, there is a multitude of different pharmacologic that can be utilized on their own or sometimes in combination with a primary care physician. Some of the most used pharmacological are baclofen, benzodiazepine, clonidine, and tizanidine. If these pharmacologic have been used poorly and are not working, the next step is for them to be administered intrathecally. This is done with a small intrathecal infusion pump that administers high doses of pharmacologic directly to a person’s central nervous system. These procedures have been done for years and have shown great success with minimal side effects. Again, this must be spoken about with your primary care physician and other specialists that your physician might refer you to.
One of the most overlooked but also effective and holistic treatments for spasticity is proper water intake. By drinking proper amounts of water daily, it helps to flush the entire system and take out lactic acid and promote better circulation and blood flow to the larger muscle groups to help reduce spasticity.
If a person with an SCI is suffering from spasticity it is suggested that they go from a holistic and non-evasive approach first and then possibly a surgical procedure last. While consulting with your primary care physician, explain how much water intake is taking place daily and if the person is receiving any type of stretching and functional movement exercise approach. If those don’t seem to be working, pharmacology can be the next appropriate step and possibly surgical intervention as a last approach to the battle against spasticity.
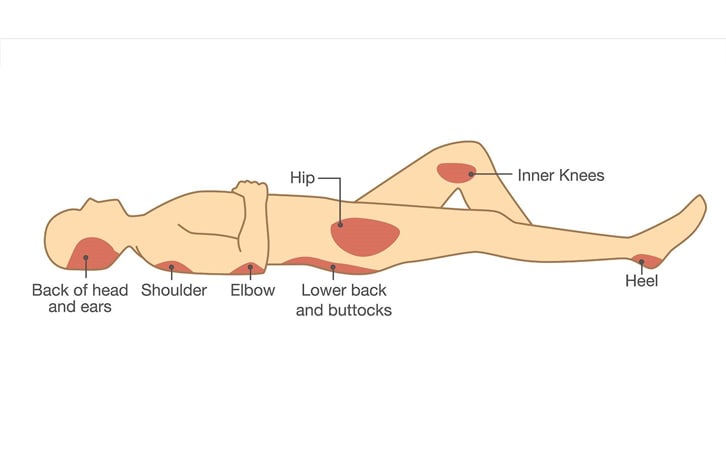
One of the most widely known secondary complications after sustaining a spinal cord injury is pressure sores/bedsores. Because of the overwhelming response emails and calls to spinalcord.com, the team has created its page which is an extremely comprehensive understanding of pressure sores, why they arise, and the prevention of future sores in the future. Nonetheless, we will elaborate further and discuss this secondary complication and provide research understanding as well.
As stated on the pressure sore fact sheet from spinalcord.com, the definition of a pressure sore that relates to spinal cord injury is: “the result of an area of skin or underlying tissue that has been damaged due to the loss of blood flow. For the skin to be healthy, it needs a constant source of blood, otherwise, it can become infected and even stop functioning completely.”
The reason why pressure sores are so prevalent after sustaining a spinal cord injury is because of a few factors. One factor that must be understood is that the person with a spinal cord injury usually has loss of feeling and/or sensation below a certain point in their body which is dependent upon the level of injury done to the spinal cord. When a person loses feeling/sensation, they do not necessarily feel that an area of skin is being irritated and therefore does not weight shift or rotate their bodies to relieve the irritated skin area. The longer the skin irritation, the quicker it causes cellular breakdown and the skin to become dead/necrotic.
Another factor to understand is that pressure sores primarily happen in bony prominent areas such as:
• elbows
• tailbone (coccyx)
• buttocks (ischial tuberosity)
• hips
• heels
• ankles
• knees
• shoulders
• back of head
There are four different stages for pressure sores/skin breakdown.
• Stage 1: the sore is not an open wound but will present a change in color and/or temperature of the skin. Upon appearance, the area will look reddened and will not blanch. In a darker-skinned person, that irritated area may appear to be a different color than what it previously looks like. The area irritated might also feel softer or firmer upon touch.
• Stage 2: the irritated area has opened or has formed visible damage to the skin at the uppermost layer called the epidermis. As the sore has expanded into deeper layers the area may now look like a blister, shallow crater or an abrasion. At this point, the skin can die off and start becoming tender or painful.
• Stage 3: the sore has extended deeper now into the subcutaneous layer and has broken through tissue, forming a crater in the irritated area. Within the opening, fat may show but not any muscle, tendon or bone.
• Stage 4: the sore has gone deeper exposing muscle, tendon or bone. At this point, damage may become irreversible and if not treated immediately, it can start causing other medical issues such as sepsis or osteomyelitis (infection in the bone).
In 2013, the National Institute of Health did a full study named comprehensive management of pressure ulcers and spinal cord injury: current concepts and future trends. Within this study, a major statistic for the spinal cord injury population stood out among the rest: “The incidence of pressure ulcers in the SCI population is 25–66%. It has also been reported that patients with higher-level spinal cord injuries are more susceptible than those with lower-level lesions. The lack of protective sensation, variable home care and access to pressure-relieving equipment, and common comorbidities (e.g. diabetes, anemia, malnutrition) contribute to the high risk for developing pressure ulcers in this population”.
To understand this statistic, it means that an astonishing 66% of individuals with SCI (whether acute or long-term) may receive some type of pressure sore. Therefore, it is so widely prevalent and known as a secondary complication that follows spinal cord injury.
Some of the most common preventative measures of pressure sores are water intake, weight management, weight shifting and movement, proper diet to increase skin integrity, cleanliness, and circulation. It is truly best for individuals with SCI to work with medical personnel (especially during the acute phase) to understand, educate and prevent pressure sores/bedsores.

A large number of spinal cord injuries are due to a major/catastrophic event (vehicular accident, slip, and fall, extreme activity, etc.). Because of this, most people affected by an SCI have to face a new way of life with a new form of disability which can be mentally and emotionally taxing. Also, when the SCI occurred, that dramatic event should never be overlooked from a mental and emotional point of view.
During the acute phase, a person with an SCI becomes focused on a survival mentality and trying to work with a large amount of medical personnel to understand everything from pharmacology, physical and occupational therapeutics, and also bowel and bladder issues. Often, the original catastrophic event is overlooked and not always addressed during the acute phase. Because of this, the person carries a tremendous amount of emotional aspects that can get buried only to cause additional grief and harm at a later date. If a person with a newfound spinal cord injury does not work with the proper mental health professional, this can stunt their emotional health and well-being as they proceed forward back into the community and society.
Spinalcord.com has put together a full fact sheet on the three different types of mental health professionals that can help a person with an SCI flourish once again. The three different types of medical professionals are therapists, psychologists, and psychiatrists. If a person with an SCI, family member or caregiver would like to understand the difference between the three different types of mental health professionals, they should refer to the fact sheet for better understanding.
Most people do not always understand that there are five stages of the coping and grieving process after a traumatic event. These five stages consist of denial, anger, bargaining, depression, and acceptance. Author Bianca Chadda of spinalcord.com does an exceptional job breaking down the 5 coping stages after a spinal cord injury.
One major study that was done by an international University named “spinal cord injury and mental health” through a health survey showed that almost half (48.5%) of the population with spinal cord injury suffered mental health issues which include depression, anxiety, clinical stress or post-traumatic stress disorder (PTSD). This statistic alone represents a substantial 56% increase over the general population and the probability of comorbidity of psychopathology. The results of the study show the vulnerability of the spinal cord injury population to emotional disorders and the importance of an individual to seek out a mental health professional. These professionals are there to assist in working on the traumatic event that has happened and the appropriate ways of moving forward with proper mental and emotional health.
Bone density or bone mineral density (BMD) is among one of the most widely overlooked secondary complications. The definition is the amount of calcium and bone mineral in bone tissue. When a person sustains a neurological issue, a good portion of the acute hospital stay is spent in a hospital bed or a sitting position. With a new paralysis injury, many factors and phases happen to the human body. Although bone density is overlooked, it is sufficient time to advocate and have a person ask for a bone density scan (bone DEXA scan) to be done by the medical team. By having a BMD scan, it will provide a baseline of the mineralization in a person’s bones. A (BMD) scan uses x-rays to measure how many grams of calcium and other bone minerals are packed into a segment of bone. The bones that are most commonly tested are in the lumbar spine, the hips (femoral neck) and sometimes they will include the forearm. When the few minute-long x-rays are complete it is then processed against the World Health Organization’s (WHO) statistical analysis for bone density. The results will explain through percentage values and it will take into consideration your age. It will then produce a report of your numbers to see if a person is at a higher fracture risk.
Osteopenia is the onset of osteoporosis and is a condition in which bone density is less for your age group and in turn, means that you are at risk of fracture.
Osteoporosis means that you are at a higher risk fracture than others in your age group. The bones have become porous and/or de-calcified.
A fact sheet done by the University of Washington states that 80% of chronic spinal cord injuries have either osteopenia or osteoporosis. That number is staggering compared to able-bodied individuals with no neurological injury. Although there is no single cause of osteopenia/osteoporosis, the University of Washington shows that there are certain causes for people with a neurological injury that they should be aware of:
• Disuse: lack of mechanical loading on the bone inhibits the stimulation of bone-building cells.
• Disordered vasoregulation: sluggish blood flow to limbs may contribute to a decrease in bone mass.
• Poor nutritional status: inadequate consumption of a healthy, well-balanced diet.
• Hormonal alterations (testosterone, PTH, glucocorticoids, calcitonin): happen as a result of SCI and play a role in the maintenance of bony formation and reabsorption.
• Metabolic disturbances in metabolites and acidity of the blood: it can influence the balance of bony formation and re-absorption.
• Autonomic nervous system dysregulation: it is caused by the injury leading to poor circulation and altered gas and nutrient exchange at the bone.
There are pharmacological and non-pharmacological treatments to assist with bone density, but there is no real cure. These treatments will help slow down the progression of osteopenia/osteoporosis and can assist in maintaining where the levels are at. Some non-pharmacological treatments are standing, functional electrical stimulation and also low-intensity vibration. A person affected with paralysis may be able to seek out an activity-based training facility to be able to assist in these non-pharmacological treatments.
Preventative measures on the University of Washington’s fact sheet are:
• consume a healthy diet
• quit smoking
• limit alcohol and caffeine intake
• stay physically fit and mentally active
• avoid falls

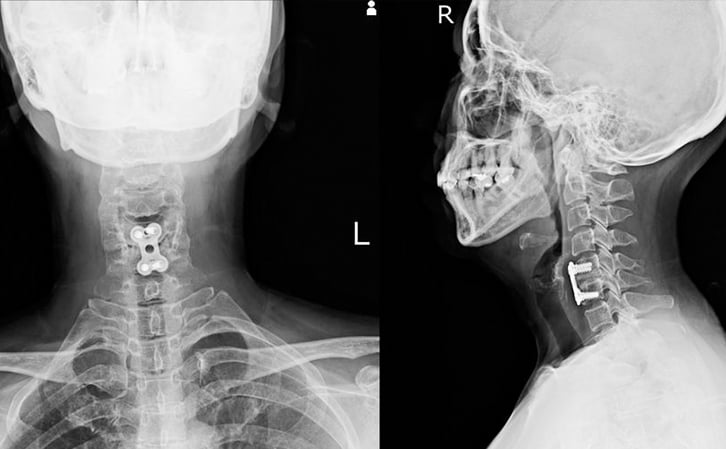
Scoliosis is a widely known medical condition/complication throughout the world. The true definition of scoliosis is a sideways curvature of the spine that occurs most often during the growth spurt just before puberty. While scoliosis can be caused by numerous conditions such as cerebral palsy and muscular dystrophy, the cause of most scoliosis is still unknown.
A great way to get a baseline understanding of scoliosis with spinal cord injury or other neurological injuries, the spinalcord.com team has created an excellent page in 2019 named “Spinal Cord Injury and Scoliosis 101”. Not only does this article do a great job of explaining the understanding of scoliosis but it also gives preventative tips as well.
One of the main factors that make scoliosis a largely recognized secondary complication of people living with a neurological injury is because of the loss of muscular control and contraction to the core muscles. Whether the person has a spinal cord injury in the thoracic or cervical area, paralysis of the core muscles (abdominals, obliques, para-spinal, etc...) becomes prevalent. Because of these paralyzed or weakened core muscles, a person tends to lean to one side. Over time, the spine starts to fixate to that certain position which is the formation of scoliosis. Even though this is a recognized secondary complication due to paralysis, there is no statistical evidence of how many adults with a spinal cord injury that has scoliosis. A large study was done by the NIH titled “Neuromuscular Scoliosis in Children With Spinal Cord Injury”. Within this study, it discloses that almost all children injured with a spinal cord injury before skeletal maturity receive some form of scoliosis. This study takes in effect the age, time of injury, area of injury and curve severity. Also, within the study, it should be noted that there were 217 pediatrics subjects and all of them had a degree curvature strong enough to be considered scoliosis.
Whether it is a child or adult with a spinal cord injury, it is best to be educated on preventative measures so to not receive scoliosis or to allow further progression of curvature in the spine. Among these preventive measures stretching and exercise to strengthen the core is very important. Other preventative measures include staying active, annual x-rays and bracing. One of the best factors to combat against scoliosis (if a person is using a wheelchair) is to get proper seating and positioning in a wheelchair. When it is time to get a manual or power wheelchair, it is strongly advised that a person should work with a certified ATP and/or SMS seating specialist. An ATP (assistive technology professional) specialist has competence in analyzing the needs of consumers with disabilities, selecting appropriate assistive technology and provide training in the use of those selected devices. An SMS (seating and mobility specialist) is a certified professional working specifically on seating, positioning, and mobility. The reason why a person would want to work with this type of specialist is to make sure that they get properly positioned in their wheelchair with enough support so that the spine does not have a way to curve for a long duration of time and create scoliosis.
If a person already has scoliosis with the curvature going past 40°, and the signs are showing that it will continue to get worse, surgery might be the only option. At this point, surgeons will most likely recommend a spinal infusion which is the ability to fuse small segments of vertebrae and can stop the curvature in certain areas of the back. This (of course), should be the last measure utilized to combat against scoliosis.
Addressed above are the most common secondary complications that are affiliated with spinal cord injury and also other neurological disorders. Although this provides a baseline understanding of each of the secondary complications, some might be feeling overwhelmed at the information, statistics and preventative measures that are mentioned. It is always best to keep in mind that a person with a neurological injury or disorder does not have to sustain one of the secondary complications by living a high quality of life. Being disciplined and educated are the key components to reducing the possibility of sustaining a secondary complication. A person with an SCI should try to build a professional relationship with their primary care physician, medical specialist, and therapist so they can always discuss with their team any signs or symptoms that they may be having. Although sustaining a spinal injury is life-changing, sustaining one of the secondary complications can be life-threatening! If a person with an SCI sees or feels symptomatic of one of these complications, they should address with their physician or medical Center as soon as possible.
.jpg)
Spinal cord injuries are traumatic for patients and their families. They cause disruptive changes to every aspect of your life and there is a lot of new information to navigate and understand. Our experts have collected everything in one place to help you learn more about your injury, locate doctors and treatment centers, find financial support, and get assistance navigating your next move.
Sponsored by Tampa personal injury lawyers at Swope, Rodante P.A. a Florida law firm located at 1234 E 5th Ave, Tampa, FL 33605.
The information provided by SpinalCord.com is not a substitute for professional medical advice, diagnosis, or treatment, see Disclaimer Policy.