MENU

- About
- Journal
- Spinal Cord Injury
- Brain Injury
- Treatment
- Legal Options
- Resources
- Local Resources
- Community
- Recognition


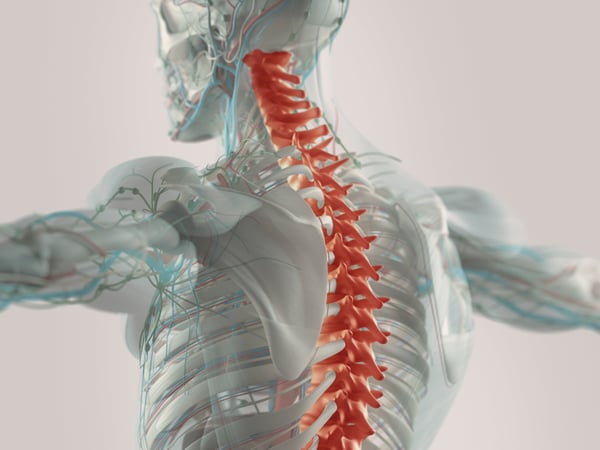
When discussing a spinal cord injury (SCI), it is usually referred to as either a complete or incomplete SCI. While both types of SCI have similar causes and symptoms, there are some key differences between complete and incomplete spinal cord injuries.
 A complete SCI is any injury that fully severs the spinal cord at the injury site. People who suffer a complete SCI lose all feeling and function for anything connected to nerves below the injury site. So, the higher up on the spinal cord an injury occurs, the more severe the symptoms tend to be.
A complete SCI is any injury that fully severs the spinal cord at the injury site. People who suffer a complete SCI lose all feeling and function for anything connected to nerves below the injury site. So, the higher up on the spinal cord an injury occurs, the more severe the symptoms tend to be.
For example, a person who suffers a complete SCI at the lower lumbar spine might lose feeling and function in their hips and legs, becoming paraplegic. A complete injury in the cervical spine (the neck) can cause someone to lose all function in their arms and legs, and they may even need mechanical assistance to breathe.
Where a complete SCI fully severs the spinal cord at the site of the injury, an incomplete spinal cord injury only partially severs the spinal cord therefore allowing some signals to pass through the level of injury.
This means that an incomplete SCI survivor might still retain some function and feeling below the site of the injury, whereas someone with a complete spinal cord injury would not have any feeling or function (because the link between the nervous system and the brain is completely severed).
There are many similarities between incomplete and complete SCIs. For example, both types of injury share many of the same causes, both impact the function of the body at and below the injury site, and therapy options for both types of injuries are often similar.
The key difference between incomplete and complete SCIs is the level of limitation they impose when both occur at the same part of the spine. Complete SCIs tend to be more limiting than incomplete SCIs. Additionally, people with incomplete SCIs generally tend to have a better overall prognosis and are able to recover faster from their injuries better than people with complete SCIs.
The location of a spinal cord injury can have an enormous impact on the severity of the symptoms caused. Generally speaking, the higher up on the spine an injury is, the more limitations it will impose.
With incomplete SCIs, however, it can be hard to predict exactly how limiting an injury may be given the different types of incomplete spinal cord injuries (more on these later). Here are some general notes about spinal cord injuries at different levels of the spine:
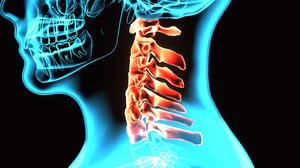 The cervical spine consists of the spinal cord and nerves located in the vertebrae of the neck. These are the C1-C7 vertebrae. There is an eighth spinal nerve section, labeled C8, which originates from the C7 vertebra.
The cervical spine consists of the spinal cord and nerves located in the vertebrae of the neck. These are the C1-C7 vertebrae. There is an eighth spinal nerve section, labeled C8, which originates from the C7 vertebra.
Injuries in the cervical spine tend to be the most limiting and immediately life-threatening of all SCIs, even among incomplete injuries. Common symptoms of cervical SCIs include paralysis of all four limbs, weakness in all four limbs, and/or loss of sensation in all extremities. Some people with C1 - C5 SCIs may lose the ability to breath without assistance temporarily or permanently.
 The thoracic spinal cord is located near the middle of the spinal column—below the cervical spine but above the lumbar spine. The vertebrae here are labeled T1-T12 by medical professionals.
The thoracic spinal cord is located near the middle of the spinal column—below the cervical spine but above the lumbar spine. The vertebrae here are labeled T1-T12 by medical professionals.
Injuries to the thoracic spinal cord generally have a better prognosis than injuries to the cervical spinal cord. Thoracic SCIs may cause paralysis in the legs, but generally leave survivors with control over their arms. This allows for a wider range of activities, such as shifting positions in a wheelchair, feeding oneself, and even driving a car with modified controls!
 The lumbar spine is located in the lower back, and consists of five vertebrae (L1-L5). However, the lumbar spinal cord is only located in the L1 and L2 vertebrae—because that is where the spinal cord itself ends. The rest of the spine merely contains spinal nerves rather than the spinal cord proper.
The lumbar spine is located in the lower back, and consists of five vertebrae (L1-L5). However, the lumbar spinal cord is only located in the L1 and L2 vertebrae—because that is where the spinal cord itself ends. The rest of the spine merely contains spinal nerves rather than the spinal cord proper.
Injuries to the L1 and L2 spinal cord segments tend to cause symptoms like weakness in the hips and legs or problems with bladder and bowel control.
 The sacral spine is the very base of the spinal column—a triangular bone at the end between the lumbar spine and the tailbone. This part of the spine contains no actual segments of the spinal cord. Instead, it houses bundles of spinal nerves that help with function in the hips, groin, thighs, and buttocks.
The sacral spine is the very base of the spinal column—a triangular bone at the end between the lumbar spine and the tailbone. This part of the spine contains no actual segments of the spinal cord. Instead, it houses bundles of spinal nerves that help with function in the hips, groin, thighs, and buttocks.
Damage to the sacral spine is relatively uncommon, but can affect bowel and bladder function, cause back and leg pain, and reduce feeling in the groin and buttocks.
There are several types of incomplete spinal cord injuries that can occur from different types of trauma. These spinal injury types are usually classified based on which part of the spinal cord the injury affected: the front, center, rear, or side.
As the name implies, this is when the center of the spinal cord is injured. Here, a loss of sensation and losing control of the limbs below the injury site is common. However, this type of injury often results in weakness in the arms more than the leg. It may be possible for some people with this type of incomplete SCI to regain some function with therapy and also with occupational/physical therapy.
Anterior cord syndrome is when the front of the spinal cord is damaged. This often interferes with sensations of touch, pain, and temperature. Most anterior cord injury survivors can recover some movement with therapy.
When damage occurs to the back (i.e. the posterior) of the spinal cord. Commonly seen with injuries caused by sharp blows directly to the back. Most posterior injury survivors maintain good posture, muscle tone, and even movement, but struggle with poor coordination.
Cauda equina syndrome is often caused by lesions in the nerve roots of the cauda equine (i.e. the lumbar spinal nerve bundle). The American Association of Neurological Surgeons (AANS) notes that cauda equina lesions can cause severe lower back pain, motor weakness, sensory loss, and even paralysis if left untreated.
Addressing the lesions can prevent more severe symptoms from developing. If treated early enough, this can prevent some permanent damage—though, as with any SCI, there is no guarantee of recovery.
Brown-Sequard syndrome is the formal name for an incomplete SCI that affects the left or right side of the spinal cord—creating an asymmetrical injury. This is the type of SCI that typically results in monoplegia/monoparesis (paralysis of one limb, typically a leg) or hemiplegia/hemiparesis (paralysis of an arm and a leg on one side of the body but results in sensation changes to pain and temperature on the opposite side of the body).
Basically, this injury may immobilize or weaken one side of the body below the injury site while leaving the other side almost fully functional.
The International Standards For The Neurological Classification of Spinal Cord Injuries (ISNCSCI) impairment scale is a method of classifying how limiting a particular condition is. The scale ranks impairment from Class A to Class E:
When doctors report on an SCI, they will often assign it one of these classifications to provide some general context about the severity of the condition.
 According to the National Spinal Cord Injury Statistical Center (NSCISC), there are roughly “17,810 new SCI cases each year” in the U.S. Across all cases of SCI, both complete and incomplete, the most prevalent causes are:
According to the National Spinal Cord Injury Statistical Center (NSCISC), there are roughly “17,810 new SCI cases each year” in the U.S. Across all cases of SCI, both complete and incomplete, the most prevalent causes are:
Epidemiology is the study of how contagious diseases are spread so they can be countered. While epidemiology is not traditionally applied to a non-contagious condition such as a spinal cord injury, studying the causes of SCIs can be crucial for preventing such injuries.
The symptoms of an incomplete SCI can vary greatly from one injury to the next because of variables like:
While symptoms can vary greatly from one case to the next, some common signs and symptoms of an incomplete SCI can include:
Some of these symptoms may cause further complications for an SCI survivor.
Therapies for an incomplete SCI can have a major impact on the prognosis for a particular injury. Generally speaking, the sooner an SCI survivor gets therapy, and the higher the quality of the therapy, the better.
Of course, every case is unique, and some incomplete SCI patients might respond better to certain types of therapies than others. Some common therapy options for an incomplete SCI include:
Getting therapy quickly after a spinal injury can have an enormous impact on the patient’s eventual recovery. Delays in seeing a doctor may result in infections, worsening of the injury, and other complications depending on the circumstances surrounding the injury.
So, the best time to see a doctor after any major trauma affecting any part of the spine is: “As soon as possible!”
If, after an accident or injury, you suspect that someone has suffered an SCI, it is important to:
After the injured person’s immediate medical needs have been taken care of and their condition has been stabilized by doctors, it may be necessary to seek legal assistance. Medical care for an SCI can be extremely costly. According to data from Statista, the average lifetime cost of an SCI for someone rendered paraplegic at age 25 is around $2,494,338 ($1,636,959 for a 50 year-old). For someone rendered tetraplegic, the total lifetime cost jumps to $5,100,941 for a 25 year-old and $2,803,391 for a 50 year-old.
This can be an insurmountable burden for many SCI survivors—especially if they lose their jobs as a result of their injury. Seeking legal assistance soon after an injury can be crucial for being able to cover the high cost of medical care.
Additionally, it is important to note that many states have a “statute of limitations” of a sort for seeking compensation for an injury. The actual time limit varies from state to state, so it is important to avoid delay while preparing a strong case—this is where a spinal cord injury attorney can help.
 Doctors may apply a variety diagnostic tests to investigate a suspected spinal cord injury. As noted by the Shepherd Center, specific tests that doctors may use to diagnose an incomplete SCI “a CT scan, MRI or X-ray. These tests will help the doctors get a better look at abnormalities within the spinal cord.” Additionally, some doctors may perform a “spinal tap” procedure to check for other problems. Here is a brief explanation of these diagnostic tests:
Doctors may apply a variety diagnostic tests to investigate a suspected spinal cord injury. As noted by the Shepherd Center, specific tests that doctors may use to diagnose an incomplete SCI “a CT scan, MRI or X-ray. These tests will help the doctors get a better look at abnormalities within the spinal cord.” Additionally, some doctors may perform a “spinal tap” procedure to check for other problems. Here is a brief explanation of these diagnostic tests:
After running a diagnosis of the SCI survivor’s injuries, a doctor may be able to provide a prognosis of the condition and a recovery plan to help the patient maintain or improve their health.
Coping with an SCI diagnosis can be incredibly difficult. Any spinal cord injury, even an incomplete one, can be life-altering. Suddenly, plans and future expectations will change—things that would be easy when in perfect health may become near-impossible after losing the use of a limb.
It will take time to cope and to relearn how to do things after a major injury. Basic tasks like eating, going to the bathroom, and getting dressed may become much more difficult and frustrating. This can quickly become emotionally draining.
Here, seeking the help of friends, family, and even other SCI survivors can prove to be invaluable. The emotional support of loved ones, and the practical advice from SCI support groups, can make adapting to life after a spinal cord injury much easier.
The road to recovery after an SCI can be a long and complicated journey. While an incomplete SCI is usually faster and easier to recover from than a complete SCI, it is still a long road.
Unfortunately, considering how varied the effects of an incomplete spinal cord injury can be, there is no “one size fits all” recovery solution. It is important to consult with a doctor to identify the best therapy options for an incomplete SCI and create a recovery plan.
In addition to the direct symptoms of an incomplete spinal cord injury, SCI survivors may experience a range of complications such as:
Some SCI survivors may experience difficult with bladder and bowel control. This can cause urinary retention, bowel or bladder incontinence,, urinary tract infections (UTIs), and other problems. Many SCI survivors use catheters and other tools to help with eliminating waste. They may also change to a high-fiber diet and set regular schedules for handling elimination to avoid potential problems.
Incomplete SCI survivors may experience abnormal feeling or numbness from their skin on their weakened or paralyzed portions of their body. This is because the connection between the nerves in the skin and the brain is damaged or severed—preventing sensation signals from reaching the brain.
This can prevent an SCI survivor from being able to feel changes in temperature, pressure, or damage like cuts.
A spinal cord injury can result in issues with the circulatory system such as changes in blood pressure, blood clots, and swelling from blood pooling in specific areas of the body (such as sores).
This can be caused by restricted movement following an SCI—pressure sores are especially common for those restricted to a wheelchair.
Some injuries that are higher on the cervical spine may actively interfere with a person’s ability to breathe by impairing control of the diaphragm or abdominal and chest muscles. In these cases, specialized breathing devices may be required.
SCI survivors with impaired breathing may also face a higher risk of developing pneumonia and other respiratory system infections.
Prolonged inactivity can cause muscles to atrophy, which can slowly cause someone with partial paralysis to lose muscle mass and tone over time. On the opposite end of the spectrum, someone with muscle spasticity (uncontrolled motion or tightening of the muscles) may experience hypertrophy (overdevelopment).
SCI survivors frequently struggle with maintaining an active lifestyle—especially immediately after their injury. Being restricted to a bed or wheelchair may lead to a more sedentary lifestyle. This, in turn, can lead to the development of sores, circulatory issues, and muscle atrophy. Engaging in physical therapy and maintaining a more active lifestyle can help improve an SCI survivor’s overall health and wellness.
Sexual dysfunction is extremely common among SCI survivors. Men may have difficulty achieving an erection while women may not be able to achieve lubrication. However, this does not necessarily preclude a healthy sex life.
For men, the use of certain medications, penile vibrators, and other assistive tools can help with erectile dysfunction. For women, exploring the use of other erogenous zones, foreplay, and lubricants can help supplement a loss of sensation in the sexual organs.
It can also help to consult with a urologist or fertility specialist to address issues with sexual function or fertility.
Incomplete SCIs can often cause abnormal sensations of pain. This is often from overused muscles, pressure sores, or partially damaged nerve connections. Depending on the cause of the pain, doctors may prescribe pain medications, physical therapy regimens, or some medical devices to help patients manage or reduce their pain.
A sudden loss of freedom of movement and ability can easily lead to depression for many SCI survivors.
For many, the support of friends and family, and even other SCI survivors, can be a crucial tool for fighting off the effects of depression. Additionally, psychiatrists may prescribe certain medications to help stabilize an SCI survivor’s mood.
Preventing spinal cord injuries requires an understanding of the risk factors that contribute to SCIs, and then taking steps to avoid or minimize those risks.
Since automobile accidents are the leading cause of spinal cord injuries, it is important to drive safely. Doing things like checking mirrors and blind spots before changing lanes, driving within the speed limit, and wearing a seat belt can all help to reduce the risk of suffering an SCI.
Remember, factors like speed, use of safety equipment, and direction of impact can all contribute to your risk of suffering fatal or debilitating injuries in an accident.
Diving accidents—particularly headfirst dives into shallow water—can easily lead to spinal cord injuries and even death. When preparing to dive into water, it is important to check the water’s depth first to confirm that there is enough room to dive safely.
Additionally, if jumping into water, it may be helpful to avoid diving headfirst to limit the risk of spine or head injury.
Falls can occur to anyone. For example, slip and fall incidents can happen while walking on a flat floor or people can fall off of ladders when trying to reach high objects or areas.
Preventing falls by keeping floors clear of clutter and spills, having help with keeping ladders stable, and avoiding walking on high and unstable surfaces can help to prevent falls at home or at work.
If playing a high-contact sport like football or hockey, it is important to wear appropriate safety equipment like helmets, padding, and gloves to prevent injuries. Even a low contact sport like baseball may require safety equipment like helmets to prevent injuries from getting hit with the ball.
According to the National Highway Traffic Safety Administration (NHTSA), “Every day, almost 30 people in the United States die in drunk-driving crashes.” The NHTSA also notes that 29% of motor vehicle traffic fatalities are caused by drunk drivers.
Being drunk impairs reaction speed, judgement, and physical coordination—all of which are important for safe driving. A drunk person is less likely to be able to brake quickly, maintain their lane, or to check their blind spots before switching lanes. They are more likely to run stop signs and red lights, which can cause a side-on crash (T-bone collision) that is more dangerous than even a head-on collision (many of a vehicle’s safety features are designed around head-on or rear-end impacts, not side impacts).
SpinalCord.com is a service that provides free and accurate information to educate the public on brain and spinal cord injuries. SpinalCord.com is sponsored by Swope, Rodante P.A., a personal injury law firm with offices at 1234 East 5th Avenue, Tampa, FL 33605 and 160 Clairemont Avenue, Suite 200, Decatur, GA 30030. The firm’s attorneys are licensed to practice in Florida and Georgia. If Swope, Rodante P.A. undertakes representation of a client, the firm may do so with the assistance of co-counsel in the state where the case is filed.
Use of this site or viewing the information contained on the site does not create an attorney-client relationship. An attorney-client relationship can only be created by a mutual agreement in writing. All information submitted through SpinalCord.com is confidential and will not be shared with any other parties. However, submitting information or transmitting materials through the site does not create an attorney-client relationship. Communications with SpinalCord.com or its recovery coaches will also not create an attorney-client relationship.
Additionally, the information relayed on SpinalCord.com does not necessarily reflect the opinions of Swope, Rodante P.A. The information on this site should not be interpreted as legal or medical advice. The majority of the content on this website was not created by lawyers or medical professionals. The information contained on this site should never be taken as a substitute for legal advice from a licensed attorney or health advice from a licensed healthcare professional.
The materials on this website are meant to be general and may not be relevant to a viewer’s individual legal or medical needs. Visitors to this website should not act on any information on this site without first seeking an opinion from a licensed attorney or licensed healthcare provider.
Laws frequently change, so the accuracy of information cannot be guaranteed.
The medical information on this site is intended to be a free resource to provide general information to the public. The information is intended to supplement instruction from your healthcare provider. The content of this website is meant for informational purposes only and is not meant to replace professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other licensed healthcare provider with any questions you may have regarding medical conditions.
SpinalCord.com does not endorse any of the companies or the opinions listed on this website. These companies and links are designed to be resources for informational use only. Additional detail about the security of your information is available at our Privacy Policy section. By submitting this form you are asking for someone from Swope, Rodante P.A. to contact you regarding your injury.
At SpinalCord.com we are committed to the protection of your privacy and we want to be upfront about how your information is collected and processed. We understand that privacy is very important to your security. Our Privacy Policy will stay up to date as new procedures are implemented. All information collected from any visitors is regarded as private information and will be kept confidential.
Every visitor to this website is recognized by our web server and it records the users domain and what pages were visited during that visitors time on the website. This method will also tell what search engine or referring site the user used to reach our website. The information obtained is used solely to increase the value of this site.
This Privacy Policy applies to our website and our subscription service. This Privacy Policy governs our data collection, processing, and usage practices. By using the website or the subscription service, you consent to the data practices described in this Privacy Policy. If you do not agree with the data practices described in this Privacy Policy, you should not use this website or subscription service.
Spinal cord injuries are traumatic for patients and their families. They cause disruptive changes to every aspect of your life and there is a lot of new information to navigate and understand. Our experts have collected everything in one place to help you learn more about your injury, locate doctors and treatment centers, find financial support, and get assistance navigating your next move.
Sponsored by Tampa medical malpractice attorneys Swope, Rodante P.A. a Florida law firm located at 1234 E 5th Ave, Tampa, FL 33605.
The information provided by SpinalCord.com is not a substitute for professional medical advice, diagnosis, or treatment, see Disclaimer Policy.